If you are tired of seeing nonstop TV Advertising on New Mexico stations promoting Medicare Part C or Advantage plans, then we have good news.
The U.S. Centers for Medicare and Medicaid Services (CMS) has issued a proposed rule that would revise regulations covering Medicare Advantage and Medicare Part D, and other Medicare programs — aiming to ban misleading television ads, promote health equity through Star Ratings of plans, and more.
How do Medicare Advantage plans work?
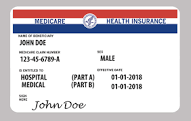
Medicare Advantage, also known as Part C, is a type of Medicare health plan that is offered by a private insurance provider through a contract with CMS, the federal agency that administers Medicare. Medicare Advantage plans take the place of what the agency calls Original Medicare — Part A (hospital insurance), Part B (medical insurance, which covers doctor visits and more), and usually Part D (prescription drug coverage). Original Medicare includes one-size-fits-all Part A and Part B, while Part D is optional and consists of many different prescription drug plans. Medicare Advantage plans may offer benefits not covered by Original Medicare, but they also come with certain potential disadvantages and risks — such as a limited network of doctors, which may be particularly challenging if you encounter unforeseen health challenges.
Original Medicare also has some distinct advantages and disadvantages. It covers every doctor and hospital in the United States that accepts Medicare, so you’re not limited to a certain network of providers. But you’re responsible for paying a deductible before coverage kicks in, and even after that, you’ll need to pay 20% coinsurance for many health services. If you’re enrolled in Original Medicare, you can buy supplemental coverage to help pay for out-of-pocket costs.
Proposed changes regarding Medicare Advantage plans
One of the new proposed rule changes would require Medicare Advantage plans to follow certain procedures when they require prior authorization for a medical procedure or test. That’s because CMS has reason to believe that some Medicare Advantage plans are requiring prior authorization without sound medical reasons in some cases, potentially delaying necessary care for patients. Under the new rule, Medicare Advantage plans would be required to use current, publicly available treatment guidelines when creating internal criteria for coverage and prior authorization. The doctor or other health professional who makes coverage decisions for a Medicare Advantage plan would also be required to have expertise in the field of medicine that they oversee. For example, a dermatologist couldn’t make decisions about whether an organ transplant should be covered.
Another proposed rule change would ban potentially misleading television ads about Medicare Advantage and Medicare Part D. In recent years, CMS has seen an increase in television ads for Medicare Advantage that don’t advertise a specific plan — instead, they make claims about Medicare and may use logos or imagery that suggest that the ad may be coming from the official Medicare program. The new rule would require television ads to be for a specific Medicare Advantage plan, mentioning the plan name. Other new guidelines would ban certain high-pressure sales tactics for Medicare Advantage plans and agents that sell those plans.
Under the proposed rules changes, starting in 2027, the Star Ratings program used to rate Medicare Advantage and Part D plans — which use data to rate the quality of care that enrollees in the plan can expect — will include what’s known as a health equity index. This health equity index will use data, starting in 2024 and 2025, to show that a plan made efforts to improve care for enrollees.